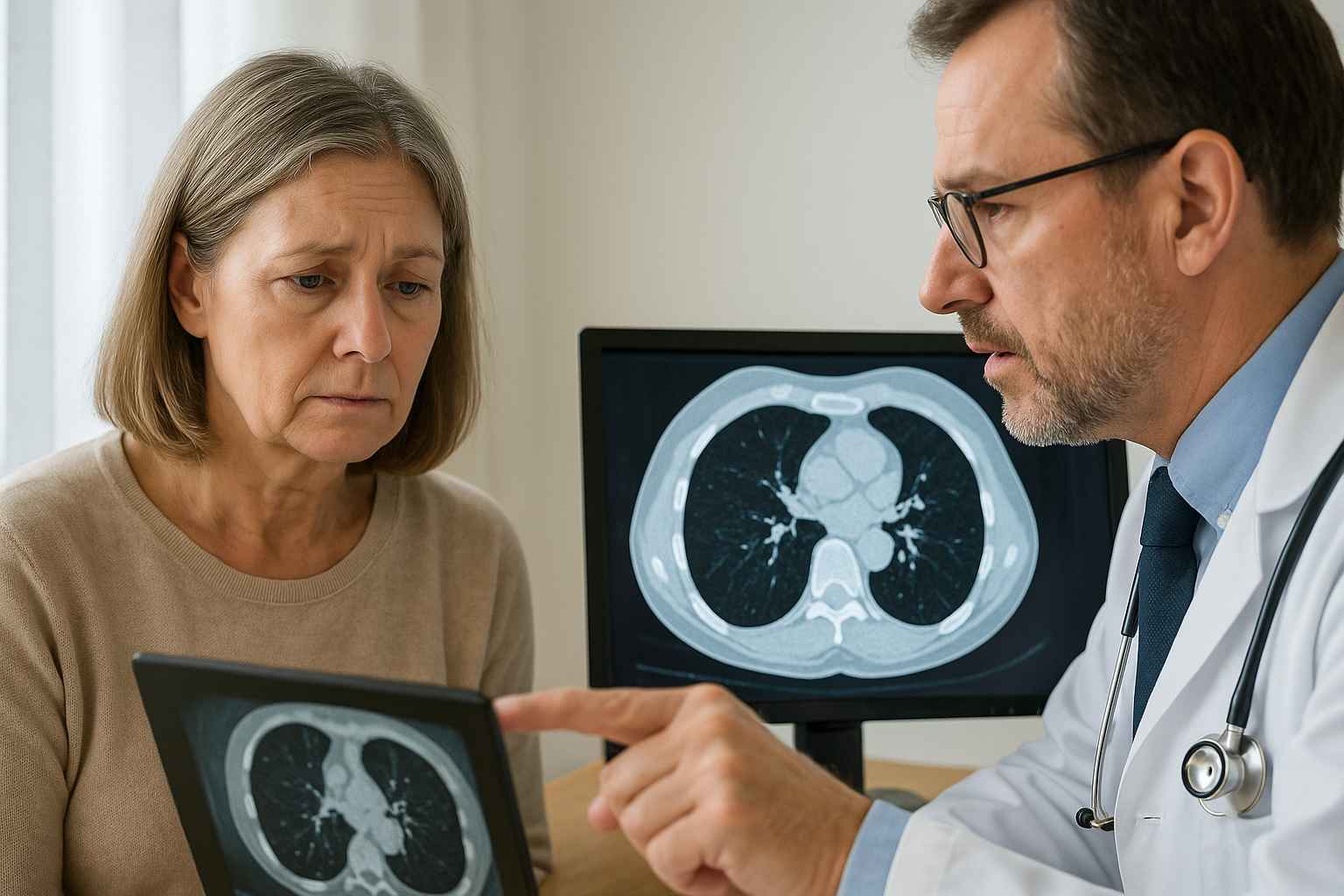
When most people hear the term “lung cancer,” they immediately think of smoking as the culprit. But what if you’ve never touched a cigarette in your life and still received that diagnosis? The reality is that non-smoking lung cancer is on the rise, and it’s baffling both patients and medical professionals.
Imagine avoiding every known risk factor—no tobacco, no secondhand smoke—and still facing a life-threatening illness. It’s like training for a marathon only to sprain your ankle at the start line. So why is this happening? And more importantly, what can you do about it?
Table of Contents
- What Is Non-Smoking Lung Cancer?
- Causes and Risk Factors Beyond Smoking
- New Research and Genetic Links to Non-Smoker Lung Cancer
- Treatments, Prevention, and Patient Advocacy
What Is Non-Smoking Lung Cancer?
Non-smoking lung cancer refers to lung cancer diagnoses in people who have never smoked or have smoked fewer than 100 cigarettes in their lifetime. While smoking remains the leading cause of lung cancer globally, nearly 15-20% of lung cancer cases in the U.S. now occur in non-smokers.
Interestingly, non-smoking lung cancer cases are often diagnosed later because patients and doctors don’t suspect cancer without a smoking history. In many of these cases, symptoms are mistaken for mild respiratory conditions like allergies or asthma, which delays detection.
While non-smokers tend to develop different lung cancer subtypes, such as adenocarcinoma, the disease remains aggressive and potentially fatal. It’s critical to understand this condition is not exclusive to smokers. In fact, it disproportionately affects women and individuals under age 50, according to American Lung Association data.
Causes and Risk Factors Beyond Smoking
If smoking isn’t to blame, what is? A growing body of research suggests several environmental, genetic, and lifestyle-related factors are contributing to this rise.
Air pollution, especially fine particulate matter (PM2.5), has been strongly linked to lung cancer in non-smokers. Long-term exposure—especially in urban areas—can damage lung tissue and trigger abnormal cell growth. Additionally, radon gas, a naturally occurring radioactive substance, is the second-leading cause of lung cancer in the U.S. and is often found in homes without detection.
Secondhand smoke also remains a significant concern. Though it’s not direct smoking, consistent exposure—especially in households or workplaces—can elevate cancer risk.
Occupational hazards such as asbestos, diesel exhaust, and exposure to industrial chemicals like arsenic or chromium are often overlooked contributors. Moreover, genetic mutations, such as EGFR (epidermal growth factor receptor) or ALK (anaplastic lymphoma kinase) gene alterations, are more frequently found in non-smokers with lung cancer than smokers.
Additionally, researchers are studying whether chronic respiratory inflammation from infections or autoimmune lung conditions could elevate cancer risk over time.
For more insights on hidden health risks, browse our top articles.
New Research and Genetic Links to Non-Smoker Lung Cancer
Advancements in genomics have brought new understanding to why non-smoking lung cancer is rising. Studies now show that many of these cancers are driven by specific genetic mutations—not environmental triggers alone.
One of the most notable discoveries is the presence of EGFR mutations in 40-60% of non-smoking Asian women diagnosed with lung cancer. In Western populations, ALK rearrangements are more common among younger non-smokers.
These genetic differences have paved the way for targeted therapies like Tagrisso (osimertinib), Zykadia (ceritinib), and Alecensa (alectinib), which are designed to attack cancer cells with specific mutations while sparing healthy tissue. This is a major leap forward from traditional chemotherapy.
Researchers are also looking into how hormonal factors, especially estrogen, might play a role in cancer development among non-smoking women. This line of inquiry could unlock more personalized treatments in the future.
Another emerging area is the role of digital pathology and AI in diagnosing these cancers earlier. AI tools trained to identify rare cancer markers may enhance early detection, especially in populations not traditionally screened.
To learn how digital marketing innovations are helping spread awareness about these developments, visit eHealthcare Solutions.
Treatments, Prevention, and Patient Advocacy
When it comes to treatment, early detection remains the most powerful tool. Unfortunately, because most non-smoking lung cancer cases are caught in the later stages, treatment often involves a combination of surgery, radiation, and immunotherapy.
Branded therapies like Keytruda (pembrolizumab) and Tecentriq (atezolizumab) are now part of first-line treatment for certain non-small cell lung cancer (NSCLC) types. These drugs stimulate the immune system to attack cancer cells, offering longer survival rates and fewer side effects than older options.
However, not all patients respond to immunotherapy. That’s why molecular testing is essential before starting treatment. It helps determine if targeted drugs or immunotherapy will be most effective.
As for prevention, indoor radon testing, reducing exposure to air pollution, and wearing protective gear in hazardous work environments are all proactive steps. While non-smoking lung cancer cannot always be prevented, increasing awareness and regular health screenings can help.
If you or a loved one is at risk, it’s essential to speak with a provider at Healthcare.pro to discuss personalized screening options.
Patient advocacy is also growing. Organizations like the GO2 Foundation for Lung Cancer and LUNGevity are amplifying voices of non-smoking lung cancer patients. They push for better screening guidelines, research funding, and removing the stigma often associated with the disease.
Conclusion
The rise in non-smoking lung cancer is more than just a medical anomaly—it’s a public health challenge that requires immediate attention. While genetic advances and targeted therapies offer hope, prevention and awareness are still the best strategies.
Understanding that lung cancer isn’t limited to smokers can change how doctors screen, how patients advocate, and how families approach care. Ultimately, recognizing the silent threats may save more lives.
FAQs
Can you get lung cancer if you’ve never smoked?
Yes, non-smoking lung cancer affects many individuals, often due to environmental factors or genetic mutations.
What are common symptoms of lung cancer in non-smokers?
Symptoms may include persistent cough, chest pain, shortness of breath, and fatigue. These are often mistaken for less serious conditions.
Are non-smoking lung cancers less aggressive?
Not necessarily. Some types may respond better to targeted therapy, but late diagnosis often makes treatment more challenging.
What types of lung cancer are common in non-smokers?
Adenocarcinoma is the most common subtype found in non-smokers, especially in women and younger individuals.
Is there a screening recommendation for non-smokers?
Currently, lung cancer screening is focused on high-risk smokers. However, people with family history or known exposures should consult a medical provider for guidance.
Disclaimer
This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.




