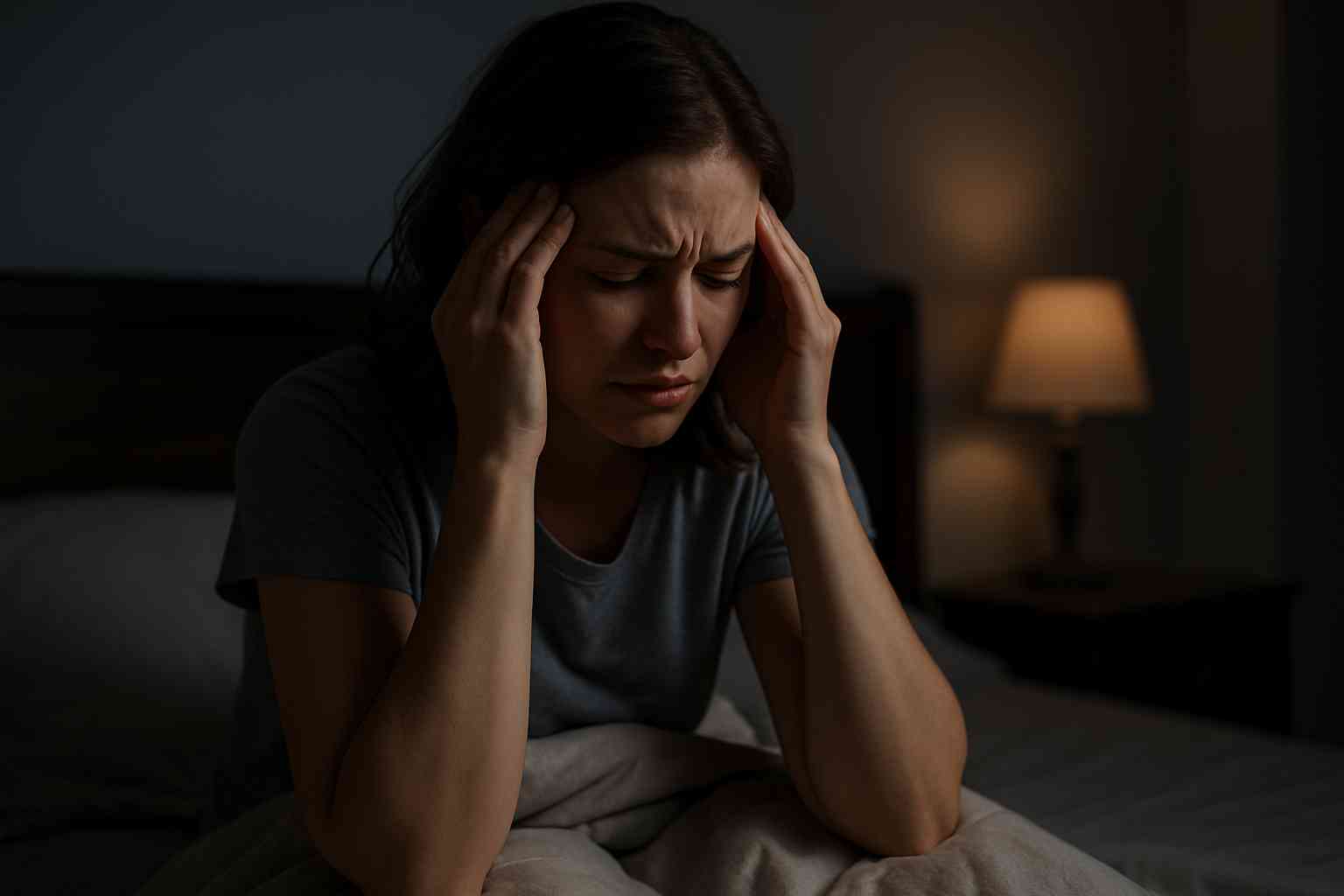
For many people living with a chronic illness, nighttime can feel like the enemy. Symptoms that seemed manageable during the day may spike just as the world quiets down. Pain intensifies, inflammation flares, fatigue deepens, and sleep often becomes elusive. But why does this happen?
You’re not imagining it. Countless people with conditions like fibromyalgia, arthritis, inflammatory bowel disease (IBD), lupus, or multiple sclerosis report worsening symptoms in the evening. This pattern is frustrating and can erode both sleep quality and emotional health.
In this article, we’ll explore the reasons behind nighttime flare-ups, from hormonal rhythms to inflammatory cycles. More importantly, you’ll find practical strategies for easing symptoms and improving rest so you can live more comfortably—even after sunset.
Table of Contents
- What Causes Symptoms to Worsen at Night?
- The Role of Sleep, Hormones, and the Immune System
- How to Manage Nighttime Flare-Ups
- Emotional Health and Evening Anxiety
- Conclusion and FAQs
What Causes Symptoms to Worsen at Night?
The evening slowdown can magnify symptoms for people with a chronic illness. During the day, distractions like work, errands, and social interactions keep your focus away from discomfort. But as the body and mind slow down, there’s more space to notice pain, tightness, or fatigue.
In some cases, it’s about circadian rhythm—your body’s internal clock. This 24-hour cycle governs hormone release, immune function, and inflammation levels. For example, cortisol, a hormone with anti-inflammatory effects, naturally decreases in the evening. With less cortisol circulating, inflammation may increase, triggering pain or swelling.
Additionally, physical activity throughout the day can lead to muscle fatigue or joint stiffness later on. If your body isn’t recovering well, minor strains or inflammation can become more pronounced at night. People with arthritis often report increased joint pain in the evening for this reason.
Digestive issues also tend to worsen after dinner. People with IBD or IBS might experience bloating, urgency, or cramping, especially if they’ve consumed trigger foods or eaten late. These physical discomforts add another layer of challenge when it’s time to wind down.
The Role of Sleep, Hormones, and the Immune System
Sleep and chronic illness are deeply intertwined. Unfortunately, they can also create a vicious cycle. Poor sleep worsens inflammation, and heightened inflammation makes sleep more difficult.
Melatonin, the hormone that helps regulate sleep, also affects immune function. Some research suggests that melatonin may increase immune activity at night, which can be problematic for those with autoimmune conditions. In these cases, the immune system might “over-activate,” leading to increased pain or fatigue.
There’s also the problem of anxiety. As the day ends, stress and worry can rise, especially if you’re anticipating a restless night. This heightened emotional state activates your sympathetic nervous system—commonly known as the fight-or-flight response—leading to racing thoughts, muscle tension, and difficulty relaxing.
Medications can contribute as well. Some drugs, like corticosteroids, may cause insomnia or jitteriness if taken too late in the day. Others may wear off before bedtime, leading to a “rebound” effect where symptoms return suddenly after temporary relief.
Understanding how your medications interact with your body’s natural cycles can help. If you’re unsure about your dosing schedule, speak to a healthcare provider or visit Healthcare.pro to find chronic care specialists.
How to Manage Nighttime Flare-Ups
While you can’t always prevent evening symptom spikes, you can take steps to reduce their severity. Managing a chronic illness requires consistency, and that includes an evening routine designed to support your body.
First, track your symptom patterns. Use a journal or app to note when flare-ups occur, what you ate, how much you moved, and what you felt emotionally. Over time, you may notice trends that allow for preemptive adjustments.
Next, practice gentle wind-down techniques. Light stretching, meditation, warm baths, or deep breathing can relax the body and mind. Avoid screens for at least 30 minutes before bed, as blue light can suppress melatonin production.
Nutrition also plays a role. Try to finish your last meal at least two hours before bed. Avoid foods known to trigger inflammation or discomfort, such as caffeine, alcohol, sugar, or spicy dishes.
If pain is your primary issue, talk to your provider about time-released or long-acting medications that provide overnight relief. For example, some patients with fibromyalgia benefit from taking duloxetine (Cymbalta) or pregabalin (Lyrica) at night to minimize pain and improve sleep.
Sleep hygiene matters. Keep your room cool, dark, and quiet. Stick to a consistent bedtime and wake-up time, even on weekends. For more strategies tailored to your condition, explore the chronic illness forums at Health.HealingWell.com.
Emotional Health and Evening Anxiety
Evening often brings solitude, and with it, emotions that were buried during the day. Living with a chronic illness can trigger feelings of loneliness, grief, or frustration—especially at night when distractions fade and discomfort rises.
It’s common to feel anxious about sleep itself. People with insomnia, pain, or fatigue-related illnesses sometimes dread bedtime, fearing they won’t rest or will wake frequently. This anticipatory anxiety can worsen sleep problems and symptoms alike.
To combat this, incorporate calming rituals and set boundaries around media consumption. News, social media, or stressful conversations can elevate cortisol and keep you alert long after the lights are off.
Talking with a therapist or joining a support group can also help process emotions. Cognitive behavioral therapy for insomnia (CBT-I) is one of the most effective interventions for people with sleep disturbance and chronic pain. This therapy teaches tools for managing thoughts, behaviors, and beliefs that interfere with rest.
Apps like Calm, Insight Timer, or Headspace can offer guided meditations, soundscapes, or sleep stories. These tools provide soothing options when silence feels overwhelming.
Remember, addressing the emotional toll of illness isn’t just about feeling better—it’s about healing holistically.
Conclusion
Living with a chronic illness is already a full-time job. When symptoms worsen at night, it can feel like there’s no off switch. But you’re not powerless. By understanding your body’s rhythms, prioritizing sleep hygiene, and creating a supportive nighttime routine, you can minimize discomfort and improve your quality of life.
Evening flare-ups are common, but they are also manageable. With the right tools, care team, and mindset, you can take back your nights—and your peace.
For more support, tools, and articles on managing chronic illness, visit Health.HealingWell.com.
FAQs
Why do my chronic illness symptoms get worse at night?
Circadian rhythms, reduced cortisol levels, and increased immune activity at night can cause symptoms to intensify. Stress and lack of distraction may also amplify awareness of discomfort.
Can better sleep help reduce chronic illness symptoms?
Yes. Quality sleep helps regulate inflammation, improve mood, and support immune function. Poor sleep often worsens pain, fatigue, and emotional health.
What medications can help with nighttime symptoms?
Depending on your condition, your provider may recommend long-acting medications like Lyrica, Cymbalta, or extended-release NSAIDs to provide overnight symptom control.
How can I calm nighttime anxiety related to chronic illness?
Mindfulness, cognitive behavioral therapy, calming apps, and nighttime routines can all reduce anxiety. Support groups and therapy can also offer long-term relief.
Where can I find more chronic illness resources and support?
Visit Health.HealingWell.com for expert-written articles, condition-specific communities, and peer support tools.
This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.




