Chronic acid reflux can be exhausting. If you’re dealing with this condition, you know how constant heartburn, pain, and dietary restrictions can impact daily life. When lifestyle changes and medications aren’t enough, surgery for acid reflux can offer real relief. This article will guide you through the surgical options, so you know what to expect and can make the best decision for your health and comfort.
Understanding Acid Reflux
Acid reflux happens when stomach acid frequently flows back into the esophagus, causing symptoms like heartburn and discomfort. While it’s normal for some acid to escape now and then, chronic reflux, or gastroesophageal reflux disease (GERD), can damage the esophagus and affect quality of life.
When is Surgery Needed for Acid Reflux?
Surgery isn’t the first step for acid reflux treatment. Most people start with lifestyle changes or medications, like proton pump inhibitors (PPIs). However, when medications stop working, or side effects become too much to handle, surgery can provide a more permanent solution.
Types of Acid Reflux Surgery
There are a few different surgical options to treat acid reflux, each suited to varying needs and severity levels. Here are some of the most common procedures.
Nissen Fundoplication: A Common Option
Nissen fundoplication is a popular procedure for acid reflux. The surgeon wraps the top of the stomach around the lower esophagus, creating a barrier that prevents acid from escaping. Many patients find long-lasting relief after this procedure, making it a trusted choice among surgeons.
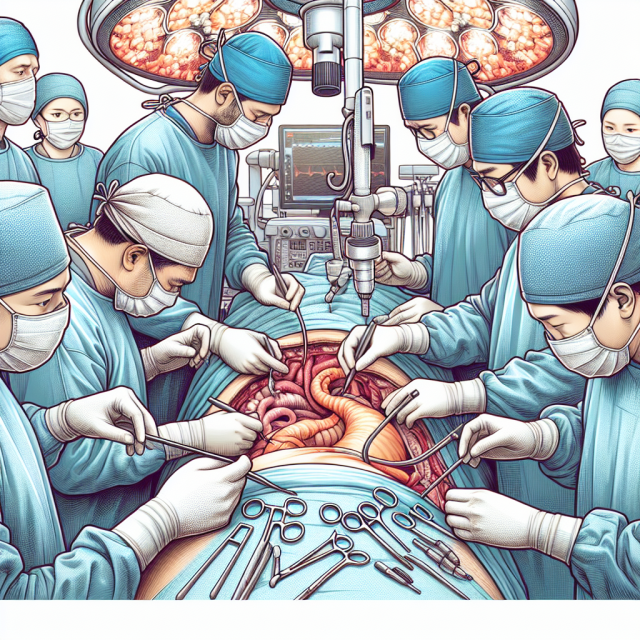
Laparoscopic Surgery for Faster Recovery
Most acid reflux surgeries, including fundoplication, are performed laparoscopically. This means the surgeon makes a few small incisions, which speeds up recovery time and reduces scarring. For patients, this often means less pain and a quicker return to regular activities.
LINX Device: A New Approach to Acid Reflux
The LINX Reflux Management System is a newer option for acid reflux. This device consists of a small ring of magnetic beads placed around the lower esophageal sphincter (LES). The magnetic attraction between beads keeps the LES closed, preventing acid reflux, but allows food to pass through during swallowing.
Choosing the Right Surgery for You
Deciding on the right surgical option is personal and depends on factors like your age, severity of symptoms, and overall health. A consultation with a gastroenterologist or surgeon will help you weigh the pros and cons of each option.
Preparing for Acid Reflux Surgery
Preparation for surgery includes discussions with your surgeon about medications, lifestyle changes, and specific instructions. You might need to stop certain medications or follow a special diet before the procedure to ensure everything goes smoothly.
Recovery: What to Expect
After surgery, expect some downtime. Most patients feel discomfort but gradually return to normal activities over several weeks. It’s essential to follow post-surgery guidelines, especially regarding diet, as certain foods might irritate the digestive tract while you heal.
Potential Risks and Complications
Every surgery has risks. Common risks associated with acid reflux surgeries include infection, difficulty swallowing, or gas bloat syndrome. Discussing these potential issues with your doctor will give you a complete picture of the surgery’s benefits and risks.
Life After Surgery: A New Normal
Life after surgery can mean a life free from constant heartburn and medication. Many patients find that they no longer need PPIs and can enjoy foods that once caused issues. Although some adjustments to diet might still be necessary, the relief from chronic pain is often worth it.
Talking to Your Doctor
Before making any decisions, it’s important to have an open and honest discussion with your doctor. They can help you understand if surgery is right for you and what to expect throughout the process.
Cost and Insurance Considerations
Surgery for acid reflux can be costly, so it’s essential to check with your insurance provider. Most insurance companies cover medically necessary procedures, but requirements vary. Be sure to get pre-approval if required to avoid unexpected expenses.
Conclusion
Living with acid reflux can feel like a constant battle, but surgery offers a path to relief and a return to a more comfortable life. Exploring options like Nissen fundoplication or the LINX system can help you regain control of your health. Remember, you’re not alone in this journey, and options exist to help you feel better and live symptom-free.
FAQs
1. Is acid reflux surgery effective?
Yes, surgery like Nissen fundoplication or the LINX procedure can be highly effective, especially for those who no longer find relief from medications.
2. How long is the recovery time for acid reflux surgery?
Recovery varies, but most patients return to normal activities within 2-6 weeks, depending on the procedure and personal healing rates.
3. Are there risks involved with acid reflux surgery?
As with any surgery, there are risks, such as infection, bloating, or swallowing difficulties. These are typically manageable and can be discussed with your surgeon.
4. Will I still need medication after surgery?
Most patients can stop taking acid reflux medication after surgery, though some may need occasional over-the-counter antacids.
5. Does insurance cover acid reflux surgery?
Many insurance plans cover acid reflux surgery if it’s deemed medically necessary, but it’s best to check with your provider to confirm.