Table of Contents
Understanding Crohn’s Disease
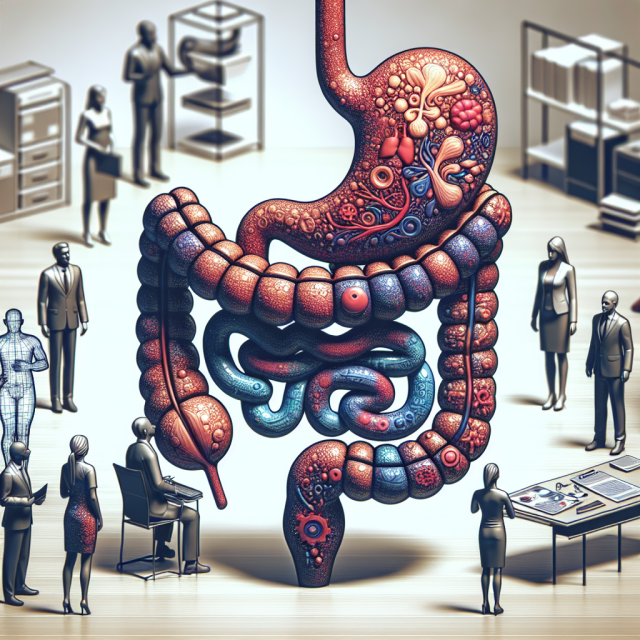
If you’ve ever experienced ongoing digestive issues, severe stomach pain, or unexplained weight loss, you may have wondered, “What is Crohn’s disease?” This chronic condition affects the digestive tract, causing inflammation, pain, and a variety of uncomfortable symptoms.
Crohn’s disease is a type of inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal (GI) tract, from the mouth to the anus. However, it most commonly impacts the small intestine and colon. Unlike temporary digestive discomfort, Crohn’s disease is lifelong and comes with flare-ups, where symptoms worsen, and periods of remission, where symptoms ease.
For those living with Crohn’s, daily life can feel unpredictable. One day, everything seems fine; the next, intense pain, diarrhea, and fatigue can take over. But with the right treatment and lifestyle adjustments, managing Crohn’s disease is possible.
What Causes Crohn’s Disease?
Doctors are still researching the exact cause of Crohn’s disease, but several factors may play a role:
1. Immune System Dysfunction
Crohn’s is believed to be an autoimmune disease, meaning the body’s immune system mistakenly attacks healthy cells in the digestive tract, leading to inflammation.
2. Genetics and Family History
If a close relative (such as a parent or sibling) has Crohn’s, you may have a higher risk of developing it. Scientists have identified specific genes linked to Crohn’s disease.
3. Environmental Triggers
While genetics play a role, external factors like stress, diet, smoking, and infections can trigger or worsen symptoms.
4. Gut Bacteria Imbalance
Research suggests that people with Crohn’s may have an imbalance in gut microbiota, which can affect digestion and immune responses.
Common Symptoms of Crohn’s Disease
Crohn’s disease symptoms can vary from person to person and may range from mild to severe. The most common symptoms include:
1. Persistent Diarrhea
Frequent, watery, or bloody diarrhea is a hallmark symptom of Crohn’s disease.
2. Abdominal Pain and Cramping
Inflammation in the digestive tract causes intense stomach pain, which can feel like a deep ache or sharp cramps.
3. Unexplained Weight Loss
Due to poor nutrient absorption and loss of appetite, many people with Crohn’s experience significant weight loss.
4. Fatigue and Weakness
Ongoing inflammation and poor digestion often lead to chronic fatigue and weakness.
5. Rectal Bleeding and Blood in Stool
Some people with Crohn’s develop ulcers in the intestines, leading to bleeding and discomfort.
6. Nausea and Vomiting
Nausea and vomiting may occur, especially if the disease has caused a narrowing or blockage in the intestines.
Diagnosis: How is Crohn’s Disease Identified?
If you suspect you have Crohn’s disease, seeing a gastroenterologist is the first step toward diagnosis. Doctors use several tests to confirm the condition:
1. Blood Tests
Blood work helps check for inflammation, anemia, or infections.
2. Stool Tests
A stool sample can detect blood, infections, or other abnormalities in the digestive system.
3. Colonoscopy and Endoscopy
These procedures allow doctors to examine the digestive tract using a small camera. Biopsies (tissue samples) may also be taken.
4. CT Scans or MRIs
Imaging tests provide detailed views of the intestines to check for inflammation, fistulas, or blockages.
Treatment Options for Crohn’s Disease
While there’s no cure for Crohn’s disease, many treatment options help reduce symptoms and prevent complications.
1. Medications
- Anti-Inflammatory Drugs (Aminosalicylates) – Reduces mild inflammation in the gut.
- Corticosteroids (Prednisone, Budesonide) – Used for short-term relief during flare-ups.
- Immunosuppressants (Azathioprine, Methotrexate) – Helps calm the immune system to prevent attacks.
- Biologic Therapies (Humira, Remicade, Entyvio) – Targeted treatments that block inflammation at the cellular level.
- Antibiotics (Cipro, Flagyl) – Used to treat infections and complications like fistulas or abscesses.
2. Dietary and Lifestyle Changes
- Low-Fiber Diet – Helps reduce irritation during flare-ups.
- Hydration – Drinking enough water prevents dehydration from diarrhea.
- Probiotics & Prebiotics – May help restore gut bacteria balance.
3. Surgery (If Needed)
For severe cases, surgery may be required to remove damaged sections of the intestine or repair strictures and fistulas.
Living with Crohn’s Disease: Coping Strategies
Managing Crohn’s disease goes beyond medical treatments. Lifestyle changes can help improve quality of life and reduce flare-ups.
1. Stress Management
Stress can worsen symptoms. Try deep breathing, meditation, yoga, or therapy to manage anxiety.
2. Support Groups and Counseling
Living with a chronic illness can feel isolating. Connecting with others through HealingWell.com can provide emotional support.
3. Keep a Food Diary
Tracking what you eat helps identify trigger foods that worsen symptoms.
4. Plan for Flare-Ups
Have a flare-up plan, including easy-to-digest meals, medications, and emergency contacts.
FAQs About Crohn’s Disease
1. Is Crohn’s disease the same as ulcerative colitis?
No. Both are types of IBD, but Crohn’s affects any part of the digestive tract, while ulcerative colitis mainly affects the colon.
2. Can Crohn’s disease be cured?
No, but with the right treatment, many people can live normal, healthy lives.
3. What foods should I avoid with Crohn’s disease?
Avoid high-fiber foods, dairy, fried foods, caffeine, and alcohol during flare-ups.
4. Does Crohn’s disease cause complications?
Yes, possible complications include fistulas, abscesses, strictures, and malnutrition.
5. Can Crohn’s disease lead to cancer?
Long-term inflammation increases the risk of colon cancer, so regular screenings are important.
For more information, visit HealingWell.com.
Disclaimer:
This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.