Table of Contents
Introduction
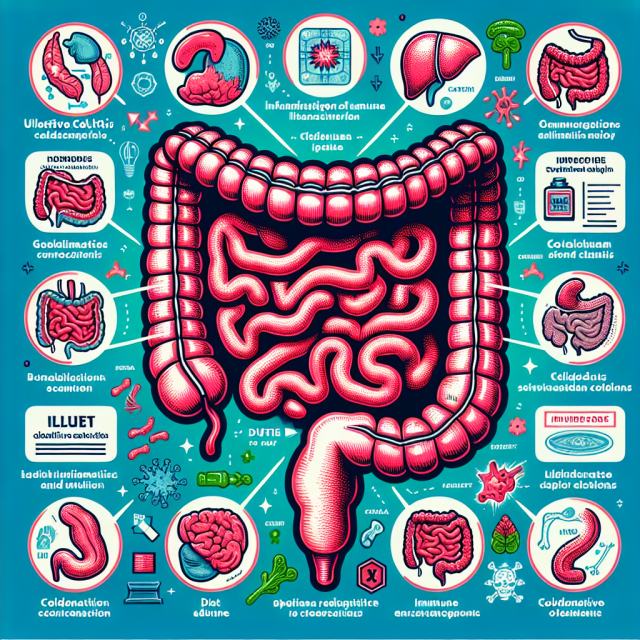
Have you ever wondered, “Why did I develop ulcerative colitis?” You’re not alone. Understanding ulcerative colitis causes can feel like unraveling a mystery. While the exact cause isn’t fully understood, research points to a mix of genetics, immune system dysfunction, and environmental factors. Let’s dive into the key insights to help you feel more informed and empowered.
What Is Ulcerative Colitis?
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that affects the lining of the colon and rectum. Unlike temporary stomach issues, this condition causes persistent inflammation, leading to symptoms like diarrhea, abdominal pain, and fatigue. Knowing what drives this inflammation is crucial to managing it.
The Role of Genetics in Ulcerative Colitis
Think of genetics as the blueprint of your body. If you have ulcerative colitis, you may have inherited certain genes that make you more susceptible. Studies suggest that having a close relative with IBD increases your risk significantly. However, genetics alone isn’t the whole story—many people with the same genetic markers never develop the disease.
How the Immune System Plays a Role
Your immune system is like your body’s personal defense team. In ulcerative colitis, this team misfires, attacking healthy cells in your gut lining instead of harmful invaders. This overreaction leads to chronic inflammation and the symptoms you experience. Researchers believe this immune response may be triggered by bacteria or viruses in your gut.
Environmental Triggers
Environmental factors often act as the spark that ignites the fire. Some of the most common triggers include:
- Smoking cessation: Interestingly, quitting smoking can sometimes precede the onset of ulcerative colitis.
- Infections: A prior gastrointestinal infection may set off the condition.
- Pollution: High pollution levels are linked to higher rates of IBD.
Although you can’t control all triggers, understanding them helps you identify potential risks.
Diet and Ulcerative Colitis
While diet doesn’t directly cause ulcerative colitis, certain foods can exacerbate symptoms. Processed foods, sugary drinks, and high-fat diets are common culprits. Adopting an anti-inflammatory diet with fresh fruits, vegetables, and omega-3 fatty acids may help manage flare-ups.
Explore more dietary tips on HealingWell’s IBD forum.
Stress and Its Impact
Stress doesn’t cause ulcerative colitis, but it can worsen symptoms. Imagine your body as a pressure cooker—stress turns up the heat, making flare-ups more likely. Techniques like mindfulness, yoga, and therapy can help manage stress effectively.
Ulcerative Colitis vs. Other IBD Conditions
It’s easy to confuse ulcerative colitis with Crohn’s disease, another form of IBD. However, the two differ in key ways:
- Ulcerative colitis affects only the colon and rectum.
- Crohn’s disease can occur anywhere in the digestive tract.
Accurate diagnosis ensures the right treatment plan.
When to Seek Medical Help
If you notice persistent diarrhea, blood in your stool, or unexplained weight loss, don’t wait. These could be symptoms of ulcerative colitis or another serious condition. Early intervention can prevent complications and improve quality of life.
Managing Life with Ulcerative Colitis
Living with ulcerative colitis means finding balance. Medications like mesalamine (Asacol) or biologics like infliximab (Remicade) can reduce inflammation and control symptoms. Complementing these with lifestyle changes ensures better outcomes. Connect with others on the HealingWell forum for support and tips.
Latest Research on Ulcerative Colitis Causes
Recent studies are delving into microbiome imbalances as a potential cause. Researchers are exploring how restoring gut flora through probiotics or fecal transplants may offer relief. These advancements bring hope for future treatment options.
Conclusion
Understanding ulcerative colitis causes isn’t just about science—it’s about empowering you to take control of your health. While genetics and immune dysfunction lay the groundwork, environmental and lifestyle factors often trigger symptoms. By working with your healthcare team and staying informed, you can manage your condition and live a fulfilling life.
FAQs
1. Can stress cause ulcerative colitis?
Stress doesn’t directly cause ulcerative colitis, but it can worsen symptoms and trigger flare-ups.
2. Are genetics the main cause of ulcerative colitis?
Genetics play a significant role, but they’re only one piece of the puzzle. Environmental and immune factors also contribute.
3. What foods should I avoid with ulcerative colitis?
Avoid processed foods, high-fat meals, and sugary drinks, as they can trigger inflammation and symptoms.
4. Can quitting smoking lead to ulcerative colitis?
Interestingly, quitting smoking has been linked to an increased risk of ulcerative colitis, though the reasons aren’t fully understood.
5. What’s the difference between ulcerative colitis and Crohn’s disease?
Ulcerative colitis affects only the colon and rectum, while Crohn’s disease can affect any part of the digestive tract.