Introduction
Have you ever wondered why a condition in the colon can make someone feel exhausted, weak, or even mentally drained? The truth is, ulcerative colitis doesn’t just impact the digestive system. It can have widespread effects on the entire body. From inflammation to fatigue and complications outside the gut, this chronic disease challenges both physical and emotional well-being.
Understanding how ulcerative colitis affects different parts of the body can help patients and caregivers better manage the disease. This article breaks down the condition’s far-reaching effects, helping individuals feel more prepared and supported on their health journey.
Table of Contents
- What Is Ulcerative Colitis?
- Digestive System Effects
- Extraintestinal Manifestations
- Long-Term Complications and Management
What Is Ulcerative Colitis?
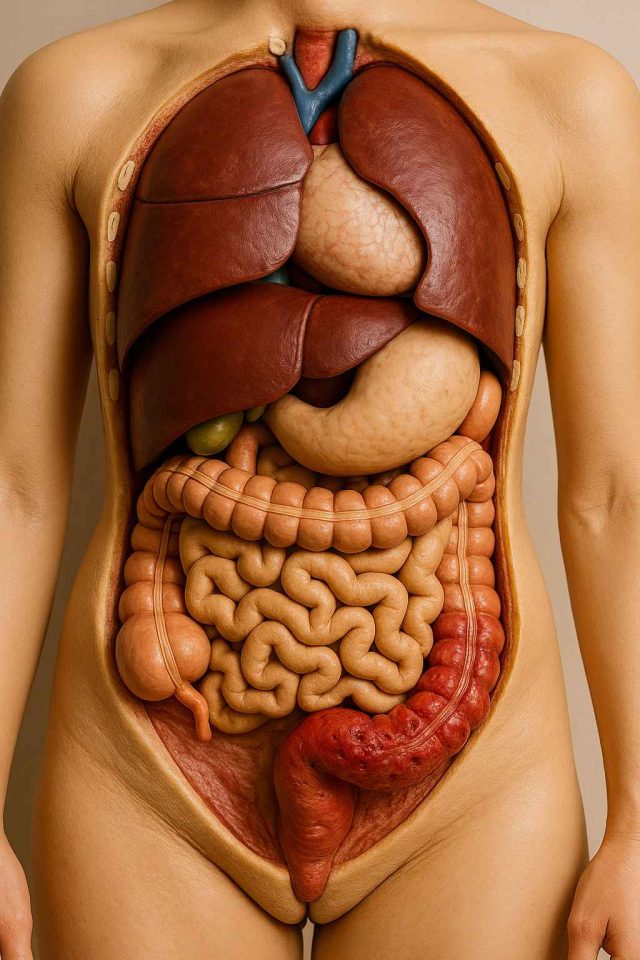
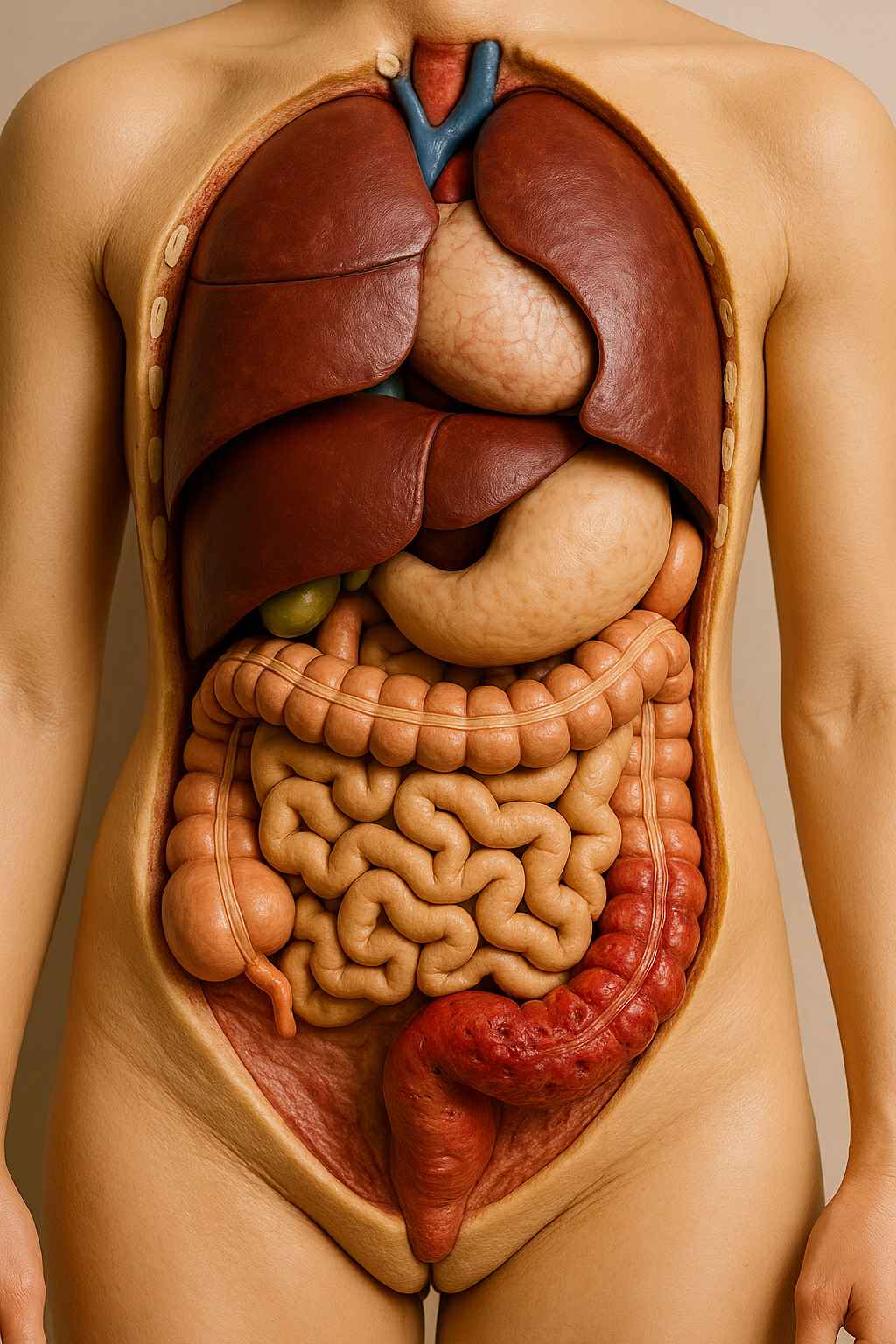
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that causes inflammation and ulcers in the lining of the large intestine, specifically the colon and rectum. It typically develops over time and can range from mild to severe. The condition is thought to result from an abnormal immune response, although its exact cause remains unknown.
Symptoms can include abdominal pain, cramping, diarrhea, blood in the stool, and a frequent urge to empty the bowel. However, ulcerative colitis is more than a digestive issue. It is a systemic condition that can lead to complications beyond the gut, especially when left untreated.
Digestive System Effects
As a disease primarily rooted in the gastrointestinal tract, ulcerative colitis has its most immediate effects on digestion. Inflammation of the colon lining leads to ulcers, reduced water absorption, and increased urgency.
Rectal Bleeding and Diarrhea
Chronic inflammation causes ulceration, which often results in blood and mucus in the stool. Diarrhea is a common symptom that can be frequent and severe, leading to dehydration and nutrient loss.
Abdominal Pain and Cramping
Patients often report cramping or a constant dull ache, especially in the lower left abdomen. This discomfort stems from the ongoing inflammation in the intestinal lining.
Malabsorption and Weight Loss
When the colon is inflamed, it cannot absorb nutrients effectively. Patients may experience unintended weight loss and vitamin deficiencies. Supplementing with iron, B12, and vitamin D may be necessary.
Colon Cancer Risk
Long-standing inflammation increases the risk of developing colorectal cancer. Regular screenings are vital for those with extensive or long-term disease.
For more information on digestive symptoms and patient experiences, visit forums at Health.HealingWell.com.
Extraintestinal Manifestations
Although ulcerative colitis primarily affects the colon, it also impacts other areas of the body. These symptoms are known as extraintestinal manifestations and can involve the joints, skin, eyes, and liver.
Joint Pain and Arthritis
Arthritis is one of the most common extraintestinal symptoms. It often affects larger joints like the knees and elbows. Inflammation in the joints may occur alongside a flare or independently.
Skin Conditions
Erythema nodosum and pyoderma gangrenosum are skin conditions associated with ulcerative colitis. The former appears as painful red nodules, usually on the legs, while the latter can lead to deep, painful ulcers.
Eye Inflammation
Conditions such as uveitis and episcleritis can cause redness, pain, and sensitivity to light. Prompt treatment is important to prevent vision issues.
Liver and Bile Duct Disease
Some patients develop primary sclerosing cholangitis (PSC), a serious condition that affects the bile ducts and may lead to liver failure. Routine liver function tests are recommended for early detection.
Mental Health Strain
Living with a chronic disease can lead to anxiety, depression, and stress. Symptoms that interfere with daily life or cause social embarrassment may worsen mental health. It’s important for patients to seek emotional support when needed.
Long-Term Complications and Management
Chronic inflammation takes a toll on the body. Without consistent management, ulcerative colitis can lead to serious complications over time.
Fatigue and Anemia
Ongoing blood loss and poor nutrient absorption can result in iron-deficiency anemia. Fatigue is often compounded by poor sleep, stress, and immune activation.
Bone Health Issues
Corticosteroids used in treatment can weaken bones, increasing the risk of osteoporosis. Patients may need bone density screenings and supplements like calcium and vitamin D.
Medication Side Effects
Long-term use of medications such as mesalamine, azathioprine, or biologics like Humira (adalimumab) and Remicade (infliximab) can lead to side effects, including infection risk, liver issues, and suppression of the immune system. Patients must be monitored regularly.
Flares and Hospitalization
Severe flares may require hospitalization or surgical intervention, including colectomy. Creating a flare management plan with your care team is crucial.
If symptoms are not well-controlled, consider seeking a specialist through Healthcare.pro, where you can find IBD-experienced providers.
Lifestyle Support
Managing ulcerative colitis involves more than just medication. Diet modifications, stress reduction, and sleep hygiene all play a role in symptom control. A personalized approach is often more effective than a one-size-fits-all model.
Conclusion
Ulcerative colitis may start in the colon, but its effects are far-reaching. From painful digestion to systemic complications, this chronic illness demands comprehensive care and attention. With the right support, patients can manage symptoms, prevent flares, and lead full lives. Staying informed, connecting with others, and working with a skilled healthcare team are essential steps toward better outcomes.
Frequently Asked Questions (FAQs)
What is ulcerative colitis?
It is a chronic inflammatory bowel disease that affects the colon and rectum, causing ulcers and digestive symptoms.
Can ulcerative colitis affect other parts of the body?
Yes. It can lead to joint pain, skin rashes, eye inflammation, and liver conditions, among other complications.
Is ulcerative colitis curable?
There is no known cure, but many patients manage symptoms effectively with medication, lifestyle changes, and support.
What treatments are available for ulcerative colitis?
Options include anti-inflammatory drugs, immunosuppressants, biologics like Humira and Remicade, and in some cases, surgery.
Where can I find support for living with ulcerative colitis?
Support communities like Health.HealingWell.com offer patient discussions and resources for coping.
Disclaimer
This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.