Medically Reviewed by Beth Hendrickson, RN
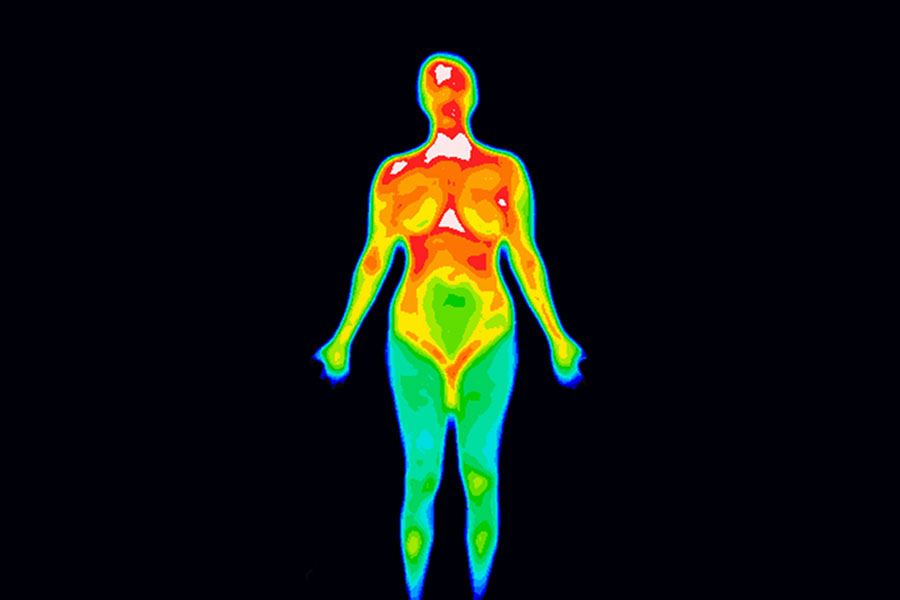
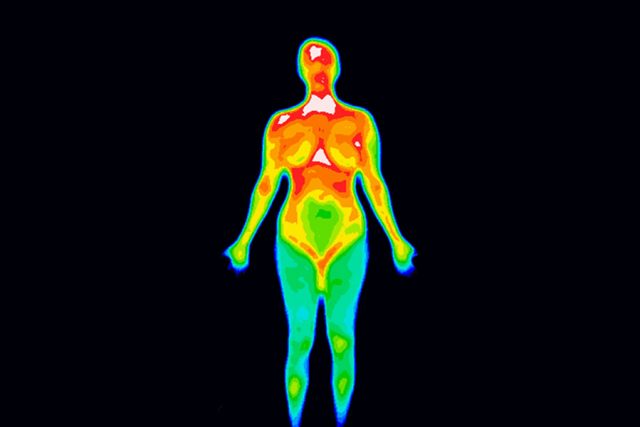
Breast thermography is a clinical diagnostic procedure which uses highly specialized infra red cameras to measure the heat coming from the body, in this case, the breast. Thermography has been approved for this purpose for many years by the US FDA (United States Food and Drug Administration) and in the past two years (2001-2002) many new doctors and technicians have entered the field. With the rise in breast thermography popularity comes the chance of your having an examination performed by non-certified or properly trained practitioners. There are also many individuals who are promoting thermography simply to build there practices, sell vitamins or other health services, and so care must be exercised when selecting a thermographic lab. Why the fuss? Because thermography is an unregulated industry with no mandatory certification requirements. This brief papers has been written to assist you in separating the what from the chaff and finding the truths behind thermal imaging.
How is Breast Thermography Performed?
It is very important that proper protocols are used when performing breast thermograms. Because thermography, or Thermal Imaging, measures heat, it is important that the patient (subject) be in a thermal “Steady-State” to insure that extraneous heat is removed from the body prior to the examination.
While different academies of thermal imaging vary to one degree or another, all have protocols which help us to obtain quality imaging, without extraneous heat on the patient or in the background of the image. Here are some examples of these protocols
The Examination Room Protocols
The room in which a thermogram is performed should be large enough to accommodate the patient, the technician, the equipment with ample room to move about the room. Thermography is performed on other body parts as well, such as arms and legs, so most labs have a room large enough for this purpose as well.
The exam room should be carpeted, there should be no windows or open doors, and if there are windows they should be properly draped and shaded to block outside light from coming into the room.
The room should be climate and humidity controlled and their should be no air blowing directly on the patient.
There should be no change in the room temperature during the time it takes to perform the examination, and the room temperature should be “comfortable” so the patient is neither perspiring or shivering, which causes thermal artifacts. Most thermogarphy labs use a 19C-23C range. These are the basic and essential protocols to be aware of.
What About Patient Protocols?
It is critical to the outcome of quality thermal imaging, that the patient be given adequate instructions and protocols prior to their examination date as there are many factors which can create false findings on the thermogram.
The patient should be given instructions at least 24 hours prior to the examination and should not do the following:
A cool bath or shower is permissible but not a hot one for at least two hours prior to the examination.
The arm pits or other parts of the body to be examined can not be shaved the day of the examination.
Beverages which contain caffeine or alcohol should not be consumed for 24 hours prior to the examination.
The use of lotions, creams, deodorant, antiperspirant, perfume or talcum powders must also be avoided.
The patient can not be sunburned, not have had chiropractic, physical therapy or massage therapy for 24 hours prior to the thermal examination, unless contraindicated by a physician.
The patient should make up a list of all medications, herbs and supplements taken that day, and should make this list available to the technician who MUST then pass this information along to the interpreting physician. You should NEVER stop taking your medications based on a thermography lab requirement without first obtaining written approval from your physician,
These are the basic protocols for the patient to follow.
How Then is the Test Performed?
You should complete standard intake paperwork about your health history, your birthing and nursing history and your menstrual cycle, sign an informed consent, and follow the protocols provided you.
You are then taken to a changing area (sometimes this is the thermographic room) where you disrobe from the waist up, including all jewelry around your neck, and you are placed in an examination gown until it is time for you to begin to acclimate. The acclimation process is simple but very, very important.
You must come to equilibrium with the temperature of the room in which the thermogram is performed so that artifact heat is not recorded in the image. This would be for example, the heat under the breast from a constrictive bra. Most all labs have the patients put their hands on top of their heads with their elbows extended outward to lift the breast and cool the arm pit region, other labs have bars for the patient to hold, Both are acceptable methods.
You will cool in the room for approximately 10-15 minutes and then images will be captured, with your arms up, of both breasts from the front, the sides, the underneath and from an angle (45 degrees also called an oblique).
After this series is completed, you are either asked to place your hands or feet in ice water, or given an ice cold gel pack to hold, for one minute. This produces a neurologic response in the breast which cools them (cancer as a rule, does not cool, healthy breasts do) and then a second set of images are made along with measurements. That’s all there is to it. You either dress and leave, or a doctor in some facilities, will give you a report of findings on the spot followed by a written report.
These are the basic and essential ingredients to a quality thermal examination of the breast
How Accurate is Thermography of the Breast?
Breast thermography is very accurate, but only in the hands of trained personnel using the correct type of thermography cameras. The accuracy of the examination varies around the world but varies from 87%-96% depending on old the literature is. The 96% reference is from 1999, the most recent published approved study. (USC Norris Cancer Center, Parisky, MD et al)
Where Can I Get More Information on Quality Breast Thermography?
It is vital, that you get good information and quality study if you are to be properly evaluated and if the thermal imaging industry is to survive the current wave of interest, and accompanying unqualified people entering the field simply to make money. Until such time as regulatory methods have been put in place, you must be careful of who performs and interprets thermographic studies.
Did you find this article helpful? Join us at HealingWell for support and information about Breast Cancer. Connect and share with others like you.
Dr. William Cockburn has been certified in clinical thermology since 1987 and is now a Fellow of the Internatinal Academy of Clinical Thermology. Dr Cockburn maintains a thermal imaging center in Los Angeles, California and has been licensed to practice since 1975. He is a graduate of the Clevaland College of Chiropractic in Los Angeles and completed post graduate training at the Los Angeles College of Law. Visit the author’s web site at http://www.breastthermography.org.