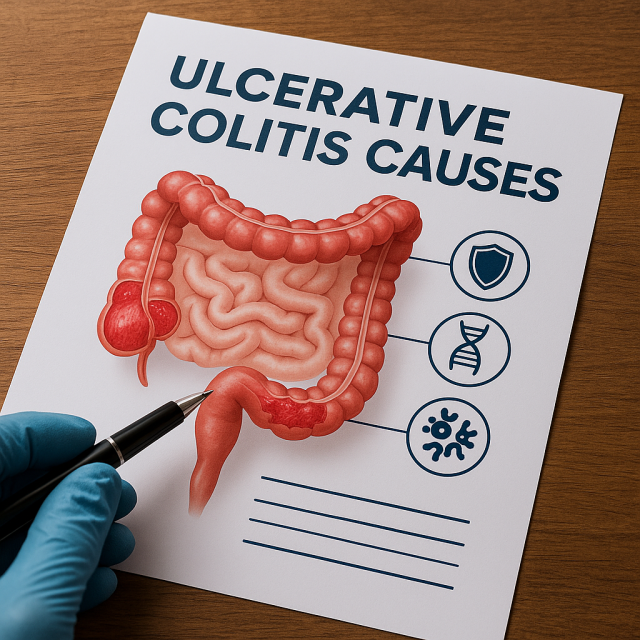
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that affects the lining of the colon and rectum. In recent years, the scientific community has uncovered compelling new evidence that is reshaping our understanding of ulcerative colitis causes. As researchers explore the complex interplay between genetics, immune response, environmental factors, and the gut microbiome, patients and healthcare providers are gaining deeper insight into how this disease begins and progresses.
Table of Contents
- Genetic Links to Ulcerative Colitis
- Environmental Triggers and Lifestyle Factors
- The Role of Gut Microbiota
- Advances in Immunological Understanding
- Conclusion
- FAQs
Genetic Links to Ulcerative Colitis
One of the most significant advances in identifying ulcerative colitis causes is the mapping of genetic risk factors. Genome-wide association studies (GWAS) have uncovered more than 200 gene loci linked to IBD, many of which are specific to ulcerative colitis. These genetic markers help explain why some individuals are more susceptible to UC than others, especially if they have a family history of the condition.
Interestingly, recent findings indicate that certain genes, such as HLA-DRB1 and IL23R, are associated with the regulation of immune responses in the gut. These genes play a role in how the body distinguishes between harmful pathogens and harmless intestinal bacteria. Mutations in these genes may lead to inappropriate immune reactions, triggering chronic inflammation in the colon.
However, genetics alone cannot fully account for ulcerative colitis development. In fact, even among identical twins, the concordance rate for UC is only about 10-15%, indicating that additional factors contribute significantly to disease onset.
Environmental Triggers and Lifestyle Factors
While genetics provide the foundation, environmental exposures often act as catalysts for disease manifestation. Researchers now believe that lifestyle and environmental factors are equally important in determining ulcerative colitis causes. For example, a Western-style diet rich in fats, sugars, and low in fiber has been linked to an increased risk of UC. These dietary patterns can disrupt the gut barrier and promote inflammatory responses.
In addition, stress, antibiotic overuse, and pollution have emerged as potential environmental risk factors. Smoking, which has a protective effect in UC (unlike Crohn’s disease), further complicates the landscape of disease triggers. Although the exact mechanism remains unclear, nicotine may suppress inflammatory pathways in the colon.
Moreover, socioeconomic status and urban living conditions correlate with higher UC incidence. These associations suggest that modern environments may expose individuals to new triggers or reduce beneficial microbial exposures that historically provided immune system training.
For more lifestyle-related insights and updates, visit Health.HealingWell.com Top Articles.
The Role of Gut Microbiota
Another groundbreaking area of research focuses on the gut microbiome. In healthy individuals, the gut is home to trillions of microorganisms that contribute to digestion, immune modulation, and barrier protection. However, in people with UC, this microbial community becomes imbalanced, a condition known as dysbiosis.
Emerging studies suggest that ulcerative colitis causes may involve a reduction in microbial diversity and a proliferation of pro-inflammatory species like Escherichia coli. Conversely, beneficial bacteria such as Faecalibacterium prausnitzii are often depleted in UC patients. This imbalance may compromise the gut lining and increase permeability, allowing harmful substances to activate immune responses.
Moreover, researchers are examining how early-life exposures, such as mode of birth, breastfeeding, and antibiotic use, affect microbiome composition and long-term IBD risk. These findings highlight the need for strategies that restore healthy microbial balance through diet, prebiotics, probiotics, or even fecal microbiota transplantation.
To seek guidance on managing your microbiome and gut health, visit Healthcare.pro.
Advances in Immunological Understanding
One of the most dynamic areas of UC research involves the immune system. Traditionally, ulcerative colitis was viewed as a purely autoimmune condition, where the body attacks its own tissues. Today, this view has evolved. Researchers now recognize UC as an immune-mediated disorder triggered by external factors and influenced by genetics.
Recent studies have identified specific cytokines and immune cells involved in UC pathology. For example, the overproduction of interleukin-13 (IL-13) by natural killer T (NKT) cells appears to play a central role in damaging epithelial cells in the colon. This discovery opens up new treatment pathways, including monoclonal antibodies that target specific cytokines.
Furthermore, the development of biologic therapies, such as infliximab and vedolizumab, has revolutionized UC treatment by blocking immune pathways rather than merely suppressing symptoms. These drugs highlight the importance of personalized medicine in managing complex immune responses.
For more updates on digital healthcare strategies, including how pharma brands are navigating targeted treatments, check out eHealthcare Solutions.
Conclusion
Our understanding of ulcerative colitis causes is advancing rapidly thanks to multidisciplinary research in genetics, microbiology, immunology, and environmental science. While no single cause explains every case, the interplay among these factors offers a clearer picture of how UC develops. With continued research, patients can look forward to more precise diagnostics and individualized treatments.
For ongoing insights and updates on chronic illness and digestive health, don’t forget to explore more articles on Health.HealingWell.com.
FAQs
What are the main causes of ulcerative colitis?
The primary causes include genetic predisposition, environmental triggers, immune system dysfunction, and imbalances in the gut microbiota.
Is ulcerative colitis hereditary?
While not strictly hereditary, having a close relative with UC increases your risk due to shared genetic markers.
Can diet affect ulcerative colitis?
Yes, diets high in fats and low in fiber can exacerbate inflammation, while nutrient-rich diets may help manage symptoms.
Is there a cure for ulcerative colitis?
Currently, there is no cure, but various treatments including medication and lifestyle changes can manage the disease effectively.
How does stress influence ulcerative colitis?
Stress can worsen symptoms and flare-ups by impacting immune function and gut barrier integrity.
Disclaimer
“This content is not medical advice. For any health issues, always consult a healthcare professional. In an emergency, call 911 or your local emergency services.”