Medically Reviewed by Beth Hendrickson, RN

Systemic Lupus Erythmatosus, commonly called Lupus, is perhaps the most misunderstood and misdiagnosed disease in the history of medicine. It has been called “The great imitator” because its symptoms can mimic other, more common diseases and syndromes. Let’s take a look at this debilitating and potentially deadly disease.
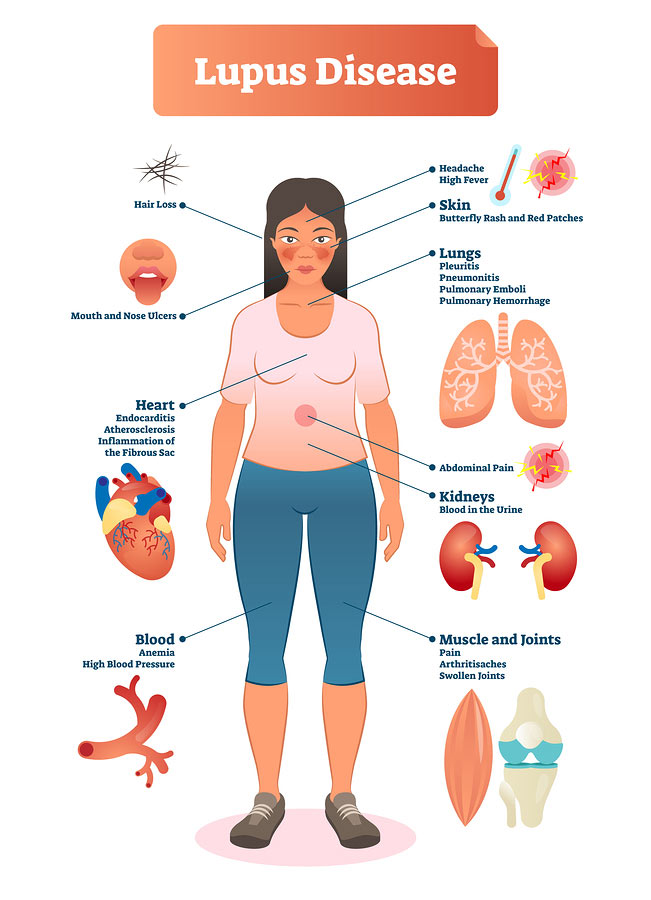
Lupus is an autoimmune disease that causes inflammation of the joints, skin, blood, and other connective tissues of the body. The immune system of the human body is designed to identify foreign cells (called antigens) such as viruses and bacteria,and develop cells to destroy these “invaders”. With lupus, the immune system cannot differentiate between antigens and the body’s own cells, and so begins to attack the cells of the connective tissues.
Anyone can have Lupus, but it is 10 to 15 more times more common in females than in males. There seem to be environmental and genetic factors that predispose an individual to Lupus, but the exact causes of the disease are unknown. Lupus tends to have a dormant, inactive stage during which the patient lives a normal, or nearly normal lifestyle. There is also an active stage, called a flare, during which the symptoms are severe, and can range from irritating to crippling.
The American Medical Association has developed a list of 11 criteria for diagnosing Lupus:
- Malar rash–a rash commonly found on the cheeks and across the bridge of the nose.
- Discoid rash–a patchy, red raised rash.
- Photosensitivity–reaction to sunlight, usually resulting in a rash.
- Oral/Nasal ulcers–usually painless, and may not even be noticed by the patient.
- Arthritis–must be present in 2 or more peripheral joints, and be non-erosive (meaning that there is no permanent damage).
- Serositis–inflammation of either the pleura (the lining of the lungs) or pericardia (the sac around the heart).
- Renal disorder–found by protein or abnormal elements such as kidney tubule cells in the urine.
- Neurological disorder–seizures or psychosis unrelated to drugs or metabolic disturbances.
- Hematological disorder– 1.) Anemia, leukopenia (a decreased white blood cell count), or lymphopenia (a decreased platelet count) on two or more occasions; OR 2.) Thrombocytopenia (a decreased platelet count) in the absence of platelet-reducing drugs.
- Immunological disorder–a positive LE prep test,a positive anti-DNA test, a positive anti-Sm test, or a false-positive syphilis test.
- Anti-Nuclear Antibodies–a positive ANA test in the absence of drugs.
Because of the variety of symptoms, a physician will need to identify at least four of these symptoms in order to diagnose Lupus. The symptoms do not have to appear concurrently. Additionally (and unfortunately), when a patient does report symptoms such as fatigue, rash, and joint pain, these telltale symptoms are often dismissed as “irrelevant”. This can (and does) lead to confusion and depression in the patient, who can be made to think, “It’s all in my head.” Most Lupus patients go through years of switching doctors, frequent hospitalizations, testing, and fighting with insurance companies before obtaining a correct diagnosis. The irony is, when a patient is told they have a debilitating, potentially fatal disease, a very common reaction is relief that they finally know what is wrong!
Thankfully, modern medicine is changing things for the better. It is estimated that between 1.4 and 2 million people have been diagnosed with Lupus. With proper diagnosis and treatments, 80-90% of Lupus patients will survive the disease. Treatments include good nutrition and exercise, avoidance of flare-triggering situations (such as sunlight exposure and stress), NSAIDs (medicines such as Motrin, Advil, and aspirin), corticosteroid therapy, and anti-malarial therapy.
With more and more information being available to assist with diagnosing Lupus, and more treatments being found, the chances are good that, eventually, a cure will be found and Lupus will become a thing of the past.
Did you find this article helpful? Join us at HealingWell for support and information about Lupus. Connect and share with others like you.
Karyn Moran Holton is a nurse who has been diagnosed with Lupus.




