Living with ulcerative colitis (UC) can feel like a rollercoaster. With symptoms that come and go, and treatments that vary from lifestyle adjustments to medications, it’s natural to feel a bit overwhelmed. This guide offers an overview of UC, explaining its symptoms, treatment options, and tips for managing everyday life, so you can feel informed and supported.
What is Ulcerative Colitis?
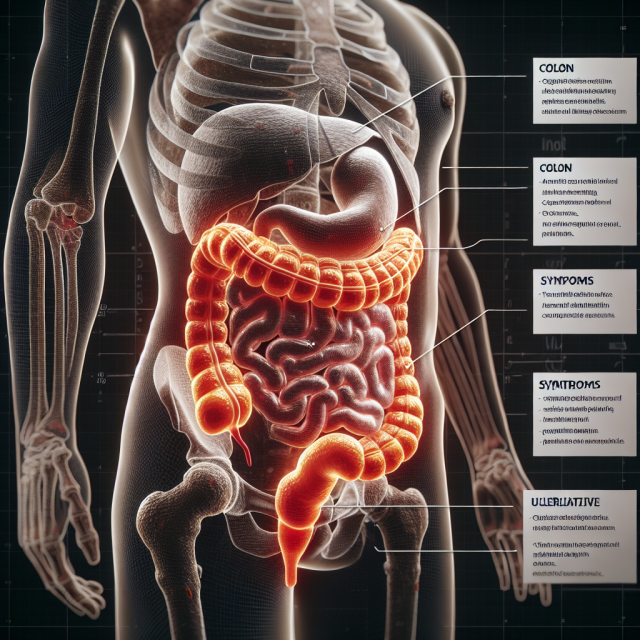
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that primarily affects the colon, causing inflammation and ulcers on the lining of the large intestine. UC is known for its unpredictable nature, with flare-ups of symptoms followed by periods of remission. Understanding this disease can make a big difference in managing it effectively.
Symptoms of Ulcerative Colitis
The symptoms of UC can range from mild to severe. Common signs include persistent diarrhea, abdominal pain, rectal bleeding, and urgent bowel movements. Many people also experience fatigue, weight loss, and anemia. For some, these symptoms are a constant companion; for others, they come in waves.
What Causes Ulcerative Colitis?
The exact cause of UC is unknown, though it’s believed to result from a combination of genetic and environmental factors. Unlike an infection, UC is not caused by bacteria or viruses. Instead, the body’s immune system mistakenly attacks the cells in the colon, leading to inflammation.
Diagnosis of Ulcerative Colitis
A UC diagnosis involves several steps, including a physical exam, blood tests, stool tests, and imaging tests like colonoscopy. These tests help rule out other conditions and determine the extent of inflammation in the colon, guiding the treatment plan.
Types of Ulcerative Colitis
There are several types of UC, categorized based on the part of the colon affected:
- Ulcerative proctitis: Inflammation is limited to the rectum.
- Left-sided colitis: Involves the rectum, sigmoid, and descending colon.
- Pancolitis: Affects the entire colon, leading to more severe symptoms.
Knowing the type of UC can help in understanding the severity and treatment options.
Medications for Ulcerative Colitis
Medications are often the first line of treatment for UC. Options include:
- Aminosalicylates (like mesalamine): These reduce inflammation in the colon lining.
- Corticosteroids: Used during flare-ups to quickly reduce inflammation.
- Immunomodulators: These suppress the immune response to help reduce inflammation.
Each medication works differently, and doctors often use a combination based on individual needs and responses.
Biologics: Targeted Therapy for UC
Biologics are newer treatments that target specific parts of the immune system to reduce inflammation. Medications like infliximab (Remicade) and adalimumab (Humira) have shown success in managing UC symptoms and achieving remission. Biologics can be a powerful tool, particularly for patients who haven’t responded to other treatments.
Surgical Options for Severe Cases
When medications and lifestyle adjustments aren’t enough, surgery may be considered. This can involve removing the colon and creating an internal pouch or ostomy. Although surgery can be daunting, it offers a permanent solution for those with severe UC and may significantly improve quality of life.
Lifestyle and Diet Adjustments
Diet plays a crucial role in managing UC symptoms. While there’s no one-size-fits-all diet, avoiding trigger foods like caffeine, dairy, and spicy foods can help. A low-fiber diet might reduce symptoms during flare-ups, while a balanced, nutritious diet is essential during remission to maintain energy and health.
Managing Flares
Managing flare-ups involves a combination of medication adjustments, rest, and stress reduction. Working closely with healthcare providers during a flare can help patients return to remission faster. It’s also helpful to have a plan in place, so patients know exactly what steps to take when symptoms worsen.
The Importance of Regular Monitoring
Regular check-ups and screenings, such as colonoscopies, are essential for monitoring UC’s progression and spotting complications early. Keeping track of symptoms and reporting them to a healthcare provider helps in fine-tuning treatment plans and maintaining overall health.
Mental Health and UC
Living with UC can take a toll on mental health. Anxiety, depression, and stress are common among UC patients. Therapy, support groups, and mindfulness practices can help manage the mental strain of chronic illness, making it easier to cope with day-to-day challenges.
Support and Resources
Having a support system is invaluable. Support groups, like those at HealingWell’s Community, provide patients and families with a place to connect, share experiences, and find practical advice. Reaching out for support can make the journey easier and less isolating.
Living with Ulcerative Colitis
Living with UC means learning to adapt. Many patients find that balancing medications, diet, exercise, and support systems is key to managing the condition. Establishing routines, planning for flare-ups, and practicing self-compassion can go a long way in maintaining quality of life.
Conclusion
While ulcerative colitis is a challenging condition, understanding its symptoms and treatment options can empower patients and their families to manage it effectively. By working closely with healthcare providers and finding the right combination of treatments and lifestyle adjustments, it’s possible to live well with UC.
FAQs
1. Is there a cure for ulcerative colitis?
No, UC is a chronic condition, but symptoms can be managed through medications, lifestyle changes, and, in severe cases, surgery.
2. Can diet alone control ulcerative colitis?
While diet plays a role, UC typically requires a combination of medication and lifestyle changes for effective management.
3. How often should UC patients have colonoscopies?
Routine colonoscopies are recommended every 1-2 years for UC patients to monitor for complications, but frequency may vary based on individual needs.
4. Do stress and anxiety worsen UC symptoms?
Yes, stress and anxiety can exacerbate UC symptoms, which is why managing mental health is important for those with the condition.
5. Are there any new treatments for UC?
Biologics and new drug therapies continue to emerge, offering more options for those with difficult-to-manage UC.
For more articles covering Ulcerative Colitis visit our Health Conditions page at health.healingwell.com/index.php/health-conditions/